In 2025, there will be an estimated 316,950 new cases of invasive breast cancer diagnosed in women; 2,800 new cases diagnosed in men, and an additional 59,080 new cases of ductal carcinoma in situ (DCIS) diagnoses in women.
One in eight women in the U.S. will be diagnosed with invasive breast cancer and one in 43 will die from the disease.
In 2025, it is estimated that 42,170 women and 510 men in the United States will die of breast cancer.
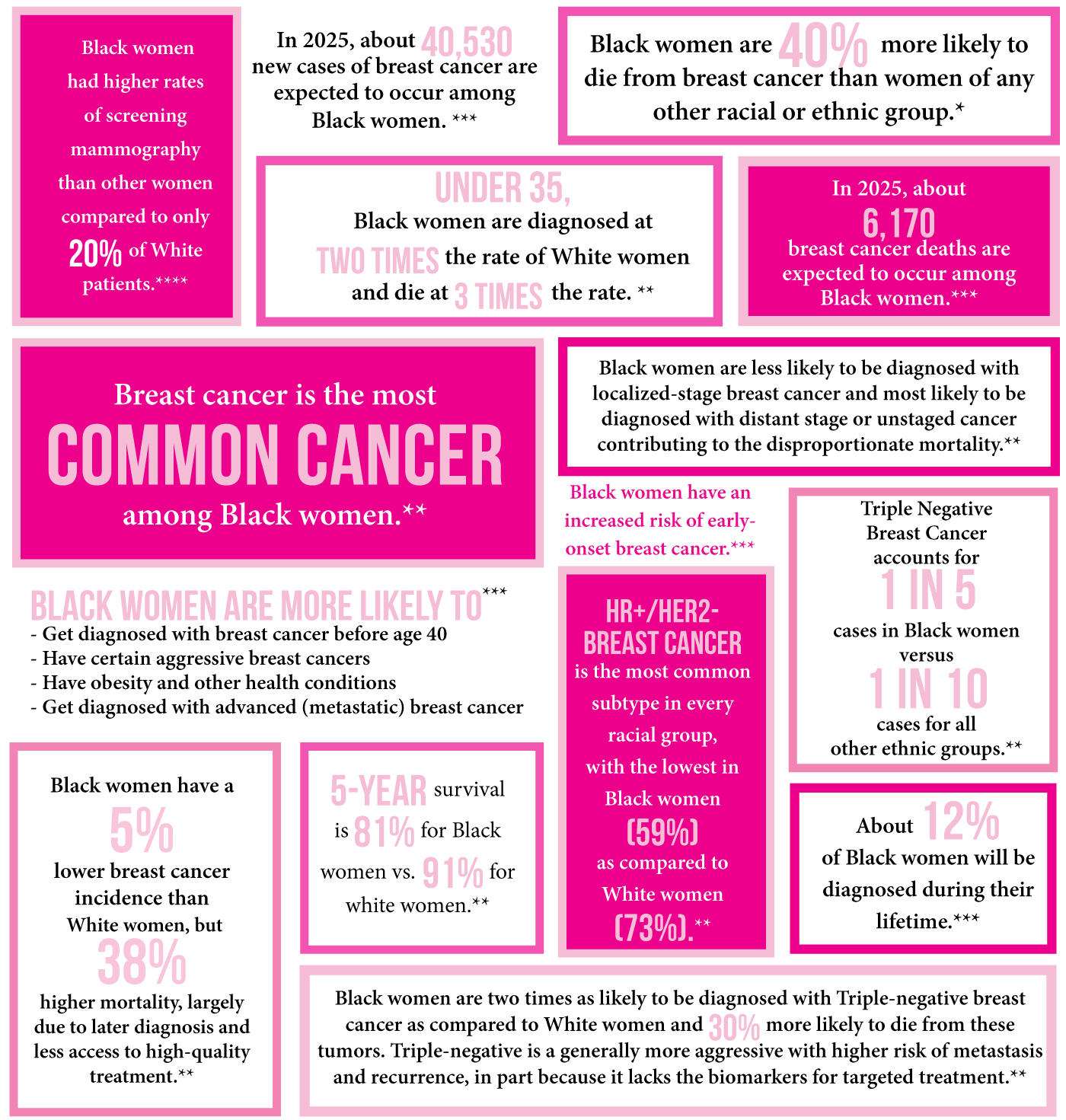
There is a breast cancer crisis in the Black community.
Sisters we must be in tune with our bodies, check our breast, know our family history and consider genetic testing. Black women under age 40 have higher rates of breast cancer when compared to White women.
Black women under 35 are two times more likely to be diagnosed with breast cancer and three times more likely to die than White women.

Black women are less likely to be diagnosed with localized-stage breast cancer and more likely to be diagnosed with distant stage or unstaged cancer contributing to the disproportionate mortality.
Black women are two times as likely to be diagnosed with triple-negative breast cancer as compared to White women and 30% more likely to die from these tumors. Triple-negative is a generally more aggressive with higher risk of metastasis and recurrence, in part because it lacks the biomarkers for targeted treatment.
Triple-Negative breast cancer accounts for 1 in 5 cases in Black women versus 1 in 10 for all other ethnic groups.
HR+/Her2- breast cancer is the most common subtype in every racial group, with the lowest in Black women (59%) as compared to White women (73%).
A rare but aggressive subtype is also more common in Black women than White women.
Breast cancer incidence and mortality vary across states due to differences in the prevalence of risk factors, screening and receipt of quality treatment.
Although overall breast cancer incidence is higher in White women than Black women, rates are higher for Black women in (Alabama, Louisiana, Mississippi and Virginia), and were not significantly different in 21 of 43 states and the District of Columbia.


Black women have statistically significantly higher breast cancer mortality than White women in every state except Colorado, New Mexico, Oregon, Rhode Island, Washington, and West Virginia, where rates are similar.
Breast cancer incidence rates are also higher among Black women than White women under age 45. The median age of diagnosis is 59 for Black women, compared to 63 for White women.
Screening mammography can detect breast cancer at an early stage, when treatment is usually less extensive and more likely to be successful.
Potentially modifiable factors that increase breast cancer risk include weight gain after the age of 18 and/or being overweight or obese (for postmenopausal breast cancer); menopausal hormone therapy (combined estrogen and progestin); alcohol consumption; and physical inactivity. There is growing evidence that high consumption of non-starchy vegetables may be associated with lower risk for hormone receptor-negative breast cancers.
For more information about breast cancer subtypes, see Breast Cancer Facts & Figures at cancer.org.



The overall 5-year relative survival rate for breast cancers diagnosed is 81% for Black women compared to 91% for White women. This difference can be attributed to both more advanced stage at detection and poorer stage-specific survival among Black women. Only about half (54% )of breast cancers in black women are diagnosed at a local stage, compared to 64% in white women.
More advanced stage at diagnosis among black women has been largely attributed to issues related to access to high-quality health care, including fewer screening mammograms, lack of timely follow-up of abnormal results, and receipt of health care at lower resourced or non-accredited facilities.

Hosting a breast health event? You are welcome to download and print copies of information about Sisters Network Inc. and other important breast cancer awareness information.
For media inquiries or general assistance, please email infonet@sistersnetworkinc.org
Contact Us